Our Individualized Programs
At DomusVi, each patient's care project is established in consultation with his/her treating physician and family. The approach in DomusVi residences aims to ensure the good health of the residents and to stimulate their maximum psychic abilities on a daily life.
The doctor specifies the organization of the resident's care based on his life history, his state of health and his degree of autonomy. The plan of care will be reassessed regularly in multidisciplinary meeting and adapted to the evolutions of its physical condition.
DomusVi’s healthcare teams accompany the resident in all aspects of his daily life. Whatever their degree of autonomy and their pathologies, they permanently ensure the quality of his care, help him in his movements and assist him if necessary during meals.

- An accepted and well-prepared entry into residence
- An attentive listening to determine together the project of life and care
- A caring team
- Non-drug therapies as much as possible
- Ongoing attention to the well-being and serenity of each resident
- A privileged dialogue with loved ones
The care approach of DomusVi is based on a simple ambition: to keep the autonomy of the residents as long as possible and to accompany each person in listening, respect and well-being.
The residence supports the overall care path of the resident: coordination of medical workers, monitoring of medical care and treatments, annual consultations (auditory, dental, ophthalmological ...), but also, the maintenance of autonomy, nutrition and hygiene. The care plan is regularly adapted according to the evolution of the state of health and autonomy of the resident.
The medical and paramedical teams organize the continuity and the security of the care. A computerized file gathers all the information of the resident's follow-up.
What is High Dependency?
The high dependency concerns mainly senior citizens affected by one of the few hundred forms of illness in which brain functions such as memory, orientation, memory and language are disrupted. Alzheimer's disease is the most common form of pathological alteration because it affects 50% of cases.
Age is the main risk factor. The risk of suffering from a pathology before 60 is minimal, but then doubles every five years or so. Some 5% of people between the ages of 70 and 79 are affected by an alteration of their general physical or mental condition. This rate rises to about 16% among 80 to 89 years old and beyond, one in three is affected.
The degeneration of the brain results in the progressive slowing down of various brain functions. Medicine distinguishes three phases. A first phase dementia, light, is manifested by the forgetfulness of recent events, mood variations, a loss of orientation in time and space or difficulties in managing the daily.
At this stage, those affected need only one-off help. In case of moderate dementia, other symptoms such as fear, anxiety, aggression, excessive reactions, hallucinations or wandering are added to the list. In the last phase of the disease, severe dementia, massive loss of intellectual and physical abilities, loss of language and limited mobility add to other symptoms. Affected people become dependent on care. The disease lasts on average between eight and ten years. Dementia is the third leading cause of death after cardiovascular disease and cancer. At present, dementia still can not be cured, but can be treated.
Neurodegenerative pathologies
“DomusVi has acquired a very high level of expertise in the care of dependent seniors”
Dr. Jean-François Delacroix
Medical Director DomusVi
Characterized by the gradual degeneration of neurons and dysfunction of the brain or even the spinal cord, neurodegenerative diseases affect tens of millions of people around the world. After Alzheimer's dementia, Parkinson's disease is one of the most common neurodegenerative diseases. It is defined by motor symptoms: rest trembling, slowing down of movements, rigidity... French doctor and physicist Jean-François Delacroix, expert in geriatrics, Medical Director of DomusVi and in charge of medical training within the group, explains the specificities and the approach chosen by DomusVi to best support the people affected and dependent.
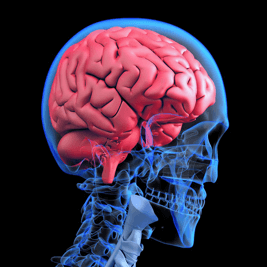
When we talk about dementia and diseases like Alzheimer's or Parkinson's, we need to talk more about neurodegenerative pathologies. The main feature is the destruction of neurons in the brain.
At DomusVi, we learned how to rethink our approach and our know-how with regard to these diseases. We must understand that psychiatric reading is wrong and that we are talking about organic diseases, just like an infarction. The French have made a lot of progress in this area, particularly in the accompaniment of patients. We can recognize that in France, we are at the forefront on the subject. The key approach is that of the heart of trades, it goes through the fundamental knowledge.
To ensure the complete management of highly dependent residents
In fact, we must be able to do our job, that is to say, beyond the actual management of the EPHAD, to ensure complete care of the highly dependent resident. Now, and this is often the problem, the management of neurodegenerative diseases is not geriatrics. It must be done, and not necessarily cheaper, because cheaper, it can lead to mischief. DomusVi can not be associated with treatments requiring average expertise. Over time, DomusVi has acquired a very high level of expertise in providing support to dependent seniors.
Dr. Jean-François Delacroix
Medical Director DomusVi
Alzheimer : A daily challenge
The German physician and neurologist Aloïs Alzheimer was the first in 1906 to describe a case of gradual dementia associated with brain damages. It took 60 years for the pathology to be considered a disease and twenty years before the researchers became interested in the patients' brains.
Alzheimer's is still a taboo disease, associated with memory disorders, while it is much more complex and carries a heavy responsibility on a daily basis. Alzheimer's disease causes progressive and irreversible destruction of neurons in the brain. It is multifactorial, with both genetic and environmental origins. Patients have two types of brain damage due to protein accumulation causing neuronal death: senile plaques (amyloid beta peptide aggregates) and neurofibrillary degeneration (accumulation of abnormal Tau proteins).
The deterioration of the neurons is manifested initially by disorders of the memory, the language, and by the loss of the recognition of the objects and the faces.
These disorders do not appear suddenly, but insidiously and slowly. They can evolve together or in isolation. The spread of lesions in the brain aggravates the symptoms: loss of cognitive and physical autonomy, behavioral disorders (apathy, depression), alteration of social interactions and isolation, degradation of vital functions.
There is currently no therapy to cure the disease. Only a few appropriate treatments and support can slow the progression of symptoms. Measures, such as the management of cardiovascular diseases, the stimulation of cognitive functions, the application of new therapies and innovative techniques, can delay entry into the disease and slow its progression.
Non-drug therapies
An absence of curative treatment does not mean that nothing can be done to improve the quality of life of the person being welcomed and those around them.
In addition to conventional medical treatments, relational support has been developed in the form of non-drug "therapies", "interventions" or "approaches". The latter play a major role at DomusVi, especially in the care of people with Alzheimer's disease or related neurocognitive disorders, as they are deemed to generate beneficial effects for the well-being of our residents. They can provide "relief" of some pain through the diversion they bring. They concern the person as well as his family or professional entourage.
The techniques of care (well-being and know-how) and non-drug therapies are one of the components of the resident's individualized care project.
Most of them answer several objectives: motricity and cognitive, cognitive and sensory, social and sensory link ...
The prerequisites of the TNM:
Qualified staff trained in geriatrics, missions:
stimulate without constraint, get to know, take into account the lifestyle and desires, prevent, maintain, relieve, enhance, reassure...
A prior assessment:
Autonomy, physical abilities, memory, self-esteem ...
Determine the individual objectives and modalities of choice of activities:
Workshop memory, therapy by singing or dancing, gardening, gentle mobilization, multi-sensory stimulation ...
The beneficial effects are different depending on the activity:
improving and/maintaining physical and cognitive abilities, reactivating communication, sensations and previous memories, easing behavioral problems, improving well-being...


